Running After a Knee Replacement
The Old Narrative I Didn’t Question at First
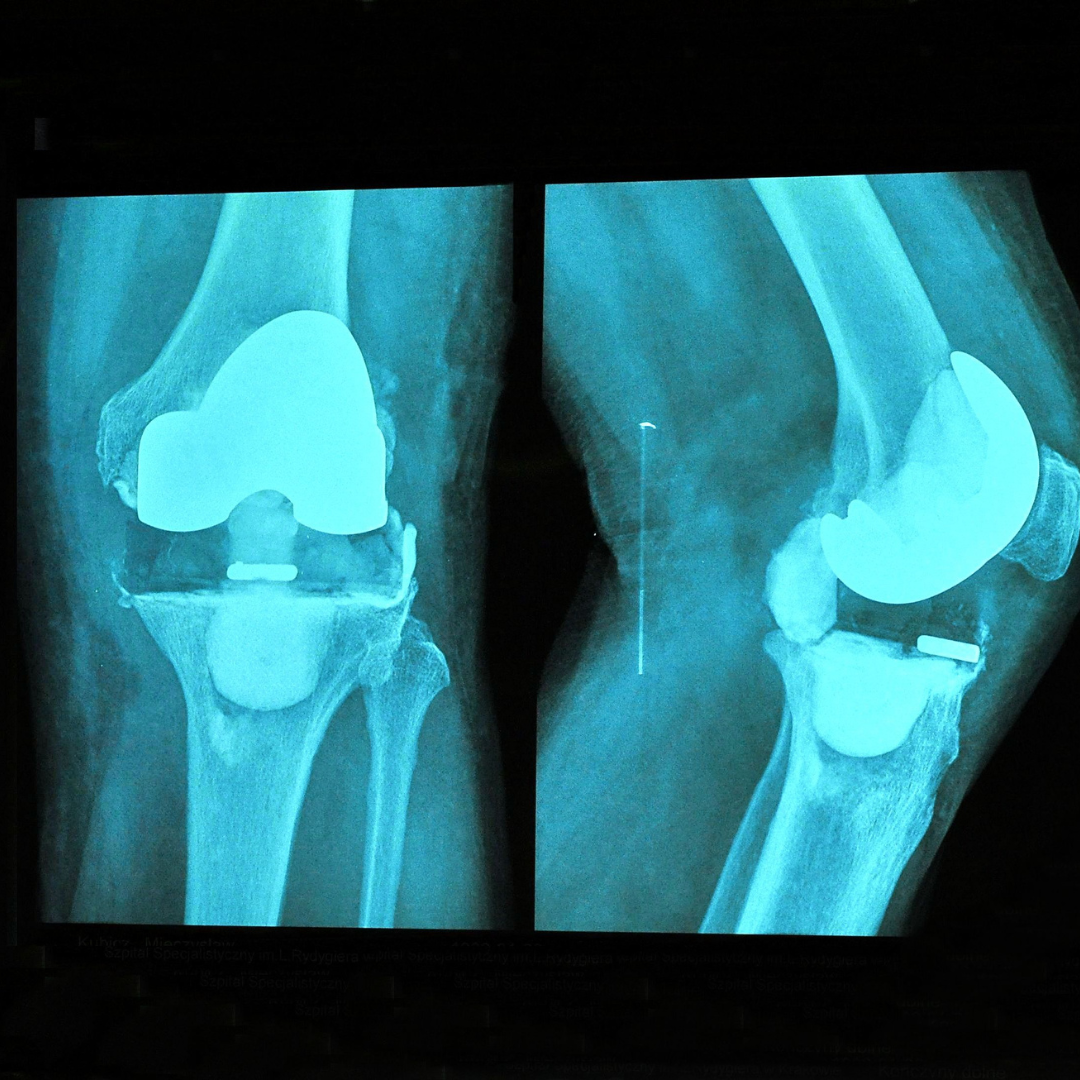
You may have been told that a knee replacement will get you back to 18 holes or a game of doubles in tennis. How about running? Forget about it. Most surgeons would have previously said “you won’t run again”. This is something I used to tell patients just hours after surgery when I was a student in an orthopedic surgery unit. I would recite the precautions from the surgery packet, “Don’t cross your legs, don’t pivot on your new knee, and DO NOT RUN!”. High impact activities were feared as they may loosen the hardware or wear it down. Why risk it? Who would want to risk needing a revision?
Insurance Doesn’t Care
I had just accepted that running was off the table after a joint replacement. In my clinicals I had only seen patients use the practice stairs in the clinic before being promptly discharged. Insurance tends to think this is the pinnacle of necessary function and typically doesn’t want to cover services beyond this point. If insurance stops covering, most people discharge from physical therapy and then stop exercising consistently. It’s scary to try and run if you don’t have guidance and need insurance to cover your treatments.
The Truth. Can people run after a knee replacement?
YES. It will be a long and slow process to get back to running after a knee replacement but it is very achievable.
Let’s dig deeper into what the research says.
Is it safe?
The research says it’s safe, but we’d like to see more. In a 2022 study, it looked at risk of revision after physically demanding activity post knee replacement. They looked at laborers and individuals who participated in “leisurely” activities that included high intensity exercise. The study DID NOT find any significant increased risk of revision with leisurely physical activity following the surgeries. The limitation of many studies like this, is that the quality of the reviewed studies were not great and so more research is needed to say this more confidently (1). With the current state of research on this topic, it may be safer to assume there is a potential risk you may shorten the lifespan of hardware by wear or loosening, but time will tell. These risks in my opinion can be mitigated with appropriate exposure to activity that improves bone quality and new growth to secure implants in cementless total knee replacements.
How long does a knee replacement last?
A study in 2019 looked at total knee replacements and unicondylar knee replacement (AKA partial knee replacement). They found that approximately 82% of total knees last 25 years and 70% of partial knees last approximately 25 years. This study did not further evaluate the activity level of the participants and thus we don’t yet know if type of activity reduces lifetime of the surgery before a revision is needed (2). With advancements in techniques and quality of materials, we think the hardware will last longer and longer in the future.
What are people getting back to?
What we have seen is that people who are active prior to surgery have a high chance of being active after surgery! In Schnieder et al (2020), they looked at return to previous level or higher level of activity following a total, partial, or patellar replacement. Partial knee replacements returned to their activities 80% of the time and total knees returned 71% of the time. This study included activities such as walking, skiing, swimming, basketball, baseball, and other sports. In Rachoy et al (2020), they found 4 runners with a total knee replacement complete the 80 kilometer Ultra-Trail du Mont Blanc.
The European Knee Association recommends sport activities after total knee replacement. These included walking, cycling, swimming, JOGGING, WEIGHTLIFTING, and more. The higher impact sports were recommended by surgeons to wait to initiate after 12 weeks to 6 months post surgery. The only sport the surgeon in this study did not recommend returning to was squash. Sorry squashers. (4)
How do you get back to running after a knee replacement?
Being active prior to surgery will increase your odds to get back to your hobbies after surgery. Maximizing strength pre surgery will give you a better starting place after you inevitably experience loss of strength and atrophy from being under the knife. Koning et al (2019) found people who maintained low-medium contact activities prior to surgery were more likely to return to the same activities.
Consistency in rehabilitation will be important to hit your milestones in range of motion, rebuilding strength, getting back to walking without an assistive device, and managing pain. Take advantage of all the time you can to rebuild your function before being discharged from PT. Following discharge, continued strengthening and building a capacity to faster and longer walking will be imperative. After some time, you will working from a leisurely walk, to a speed walk, and then a jog. The key? Graded exposure and safe progressions. The rule of 10% is typically a good idea. If you are going to progress, decide to progress volume (distance or time) or intensity (speed) by 10% week to week. It is not law, but a good practice to prevent a “too much too soon” situation that may lead you to more setbacks. Keep reading to see how one of our clients tackled this.
Case Study:
Situation
A member of the local sheriff’s office was referred to BellPT with the goal to return to running and pass the department’s fitness testing requirements. Officer “Joe” was 6 months post bilateral partial knee replacement at this time. This tall glass of water came in at 51 years of age, standing 6 foot 9 inches, and weighing in at 298 lbs. He has not run since before surgery and is uneasy to try it alone. Being an officer, the capacity to run is necessary for his own safety and those he protects.
The Unfortunate & Typical PT Experience
Joe had 4-5 week bouts of physical therapy after each surgery where he had conquered going up and down stairs and maxing out their shuttle machine (a shuttle is essentially a band resisted leg press machine). This is great progress but nowhere near ready to run or pass a fitness test. Unfortunately, this is where many clinics or insurances feel further intervention is no longer necessary.
Working With Bell Performance Therapy
When we began working with Joe, we discussed potential risks and got right into working towards running. I then made 3 points that would guide our time together.
Listen to your body, it knows best.
Reactive swelling does not equal damage and is very normal BUT is also good feedback to inform us that you aren’t ready to progress yet.
Consistency is key.
When working with Officer Joe, we began with walking a few days a week with strengthening sprinkled in when it could fit into his long work days. Here is how the next 3 months went.
Months 1-2
We began with a 20 minute walk at 3mph on the treadmill. Even this activity caused reactive swelling and required us to reduce speed or volume from day to day. One modification we made that helped reduce soreness and lessen the swelling was to add a slight incline to reduce the ground reaction forces (forces you must absorb from walking) while walking on the treadmill. This incline modification helped tons and persisted throughout our training.
We progressed to walking fartleks of 50 second slow walks with a 10 seconds quick walk at 4-4.5mph. His body informed us that this was the maximum he was able to tolerate at this time through swelling and soreness.
Month 3
At 3 months we began to tolerate the fartleks with less and less swelling. We would progress to longer duration quick walks, slight increases in speed, and overall duration following our 10% rule. We implemented greater arm swings and incorporated a “bounce” to help transition into a jog. We added in low impact plyometrics like “calf bounces” on strength days to continue to build capacity towards running.
Surprise!
At 11 weeks into the program, we are informed that Joe will have to complete his workplace fitness assessment in 1 week, something we anticipated having another 1-2 months to prepare for.
We had laid a strong foundation of capacity with some preparations for running/ jogging. Time to get ready for the races. Over the next week we progressed to ensure we could tolerate the required 300 meter run with some turns. As expected, our first attempts led to his knee swelling like a balloon but was pain free. With the confidence to meet the test cutoffs, we tapered back the last 3 days of training to manage swelling and residual fatigue.
Results
He completed the running portion with 13 seconds to spare as well as pass all other requirements including push ups, sit ups, and planks with flying colors.
In addition to passing his test, Joe experienced the other benefits of consistent exercise. He lost 16lbs in this journey as well as reduce his resting heart rate by 16 beats per minute.


Most importantly, he got a taste of what he is capable of and began to chip away at the functional ceiling the healthcare and insurance system had convinced him was everlasting.
Conclusion
A knee replacement is not a death sentence. You can get back to running and many other activities. The process is slow, it is simple, sometimes boring, but not easy.
If you are struggling to get back what you love doing, let us help guide you back to it.
*A fictional was name used in case study*
References
Additional Related Content
https://bmjopensem.bmj.com/content/6/1/e000729
https://www.sciencedirect.com/science/article/pii/S1877056820302930